Thorough Insight into Blood Test Markers Essential for Arthritis Diagnosis
Gaining a profound understanding of blood test markers for arthritis is pivotal for achieving accurate diagnoses and effective management strategies for arthritis, a prevalent condition affecting millions across the United Kingdom. These biological markers serve as crucial indicators, illuminating the existence of inflammation and autoimmune responses within the body. Such insights are invaluable in determining the type and severity of arthritis a patient may be experiencing. By enhancing our understanding of these markers, both patients and healthcare professionals can adeptly navigate the complexities of arthritis management, ultimately leading to improved health outcomes and a significantly enhanced quality of life for those affected by this debilitating condition.
Understanding the Critical Importance of Blood Test Markers in Arthritis Diagnosis
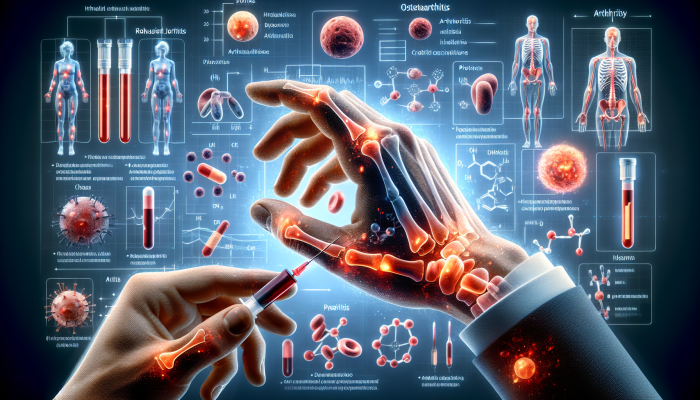
Arthritis blood test markers are biochemical substances found in the bloodstream, providing vital information about the presence and effects of arthritis on the body. These markers include a diverse array of proteins, antibodies, and other molecules that change in concentration in response to inflammation or joint damage. Their primary function is to assist in diagnosing various forms of arthritis, such as rheumatoid arthritis, osteoarthritis, and psoriatic arthritis. Each specific type of arthritis may present a distinct set of markers that healthcare professionals analyse during blood tests, making the understanding of these markers absolutely essential for accurate and timely diagnosis.
When patients exhibit symptoms commonly associated with arthritis, including joint pain, swelling, and stiffness, medical professionals frequently recommend blood tests to evaluate these markers. The results provide critical insights that assist clinicians in crafting the most effective treatment plans and tracking their effectiveness over time. It is vital to understand that while these markers yield significant diagnostic information, they must not be interpreted in isolation. Healthcare providers need to consider the patient's complete clinical picture, which encompasses symptoms, medical history, and results from other diagnostic tests, to make informed and accurate treatment decisions.
In-Depth Analysis of Different Types of Blood Test Markers for Arthritis
The range of arthritis blood test markers is extensive, incorporating numerous indicators specifically designed for various types of arthritis. For example, rheumatoid factor (RF) is routinely assessed in patients suspected of having rheumatoid arthritis. Elevated levels of RF typically indicate an autoimmune response, where the body mistakenly attacks its own tissues. Another significant marker is the anti-cyclic citrullinated peptide (anti-CCP) antibody, known for its high specificity to rheumatoid arthritis, and can sometimes be detected even before clinical symptoms manifest.
In addition to these specific markers, the erythrocyte sedimentation rate (ESR) is a well-established test performed in the UK, evaluating general inflammation levels within the body. While it is not exclusive to arthritis, an elevated ESR can suggest the presence of inflammatory processes linked to various forms of arthritis. Understanding the significance of these markers fosters a more nuanced diagnostic approach, empowering healthcare professionals to formulate treatment strategies that address the specific type of arthritis affecting the patient.
The Indispensable Role of Regular Testing in Successful Arthritis Management
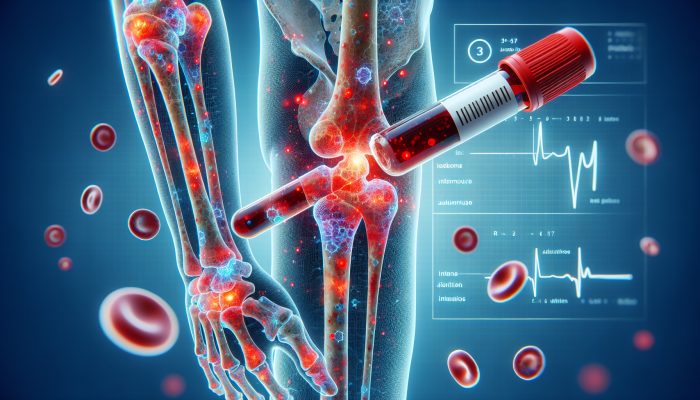
Consistent testing for arthritis blood test markers is essential for both initial diagnosis and the ongoing management of the condition. Given that arthritis can be progressive, monitoring these markers enables healthcare providers to observe changes in a patient’s condition over time. Routine blood tests empower clinicians to assess the effectiveness of treatments, permit necessary adjustments, and identify potential complications early, which is critical for preserving joint health and enhancing overall wellbeing.
Patients in the UK are strongly encouraged to maintain transparent communication with their healthcare providers about the frequency of testing. For certain individuals, it may be advisable to undergo testing every few months, particularly during the early phases of treatment or when symptoms fluctuate. Regular monitoring ensures that any increases in inflammatory markers are promptly addressed, potentially averting further joint damage and significantly improving the quality of life for individuals living with arthritis.
Interpreting Results from Arthritis Blood Tests: A Comprehensive Guide

Interpreting the results of arthritis blood tests necessitates a nuanced understanding of the levels and patterns of various markers. Normal levels can vary significantly among individuals, meaning that what may be elevated for one person might not be for another. Therefore, it is essential to consult with a knowledgeable healthcare professional who can contextualise these results within the broader framework of the patient’s overall health status, including lifestyle factors and medical history.
For instance, if a patient's rheumatoid factor levels are elevated but they do not display symptoms typically associated with rheumatoid arthritis, further investigation may be warranted to rule out false positives or other underlying conditions. Similarly, correlating blood test results with clinical symptoms is vital for achieving an accurate diagnosis. A thorough assessment by a rheumatologist can lead to a clearer understanding of what the test results mean for the patient's treatment plan and overall health strategy.
Identifying the Limitations of Arthritis Blood Test Markers
While arthritis blood test markers provide invaluable insights, they are not without limitations. One significant drawback is that some markers may be present in individuals without arthritis or may not be elevated in every case of the disease. This variability underscores the importance of using these tests alongside other diagnostic methods, such as imaging studies and physical examinations, to create a comprehensive view of the patient’s condition and requirements.
Moreover, some patients may display symptoms of arthritis without corresponding changes in blood test markers, posing challenges for healthcare professionals. In such instances, clinicians may need to rely on clinical judgement and patient history to reach a diagnosis. Consequently, while arthritis blood test markers are essential tools in the diagnostic arsenal, they should be integrated into a broader diagnostic strategy rather than solely relied upon for clinical decisions.
Key Blood Test Markers Utilised for Arthritis Diagnosis Across the UK
In the UK, various blood test markers are routinely employed to diagnose and monitor arthritis. Developing a thorough understanding of these markers can empower patients, enabling them to engage more effectively in their healthcare journey and ensuring they are well-informed about the tests pertinent to their condition.
Rheumatoid Factor (RF): A Vital Indicator for Arthritis Diagnosis
Rheumatoid factor (RF) is one of the most frequently tested markers in the UK for diagnosing rheumatoid arthritis. This autoantibody can be detected in the bloodstream and is often linked to the presence of inflammation and joint damage. Elevated RF levels may indicate an ongoing autoimmune process that contributes to the destruction of joint tissues.
However, while RF is a significant marker, it is crucial to comprehend that it is not exclusively indicative of rheumatoid arthritis. Elevated RF levels can also manifest in other conditions, such as Sjögren's syndrome, and even in some healthy individuals. Thus, a positive RF test should be interpreted cautiously and always in conjunction with clinical symptoms and additional diagnostic tests. In the context of ongoing monitoring, any fluctuations in RF levels can provide valuable insights into treatment effectiveness and disease progression, assisting healthcare providers in adapting their treatment strategies as necessary.
Anti-Cyclic Citrullinated Peptide (Anti-CCP): A Significant Indicator for Early Detection
The anti-cyclic citrullinated peptide (anti-CCP) antibody acts as another essential marker for diagnosing rheumatoid arthritis. This antibody is highly specific to the condition, making it a more definitive indicator compared to RF. The presence of anti-CCP antibodies can sometimes be detected years before the clinical onset of rheumatoid arthritis, presenting a vital opportunity for early intervention that can significantly influence long-term outcomes.
In practical terms, testing for anti-CCP antibodies can lead to more accurate diagnoses, allowing healthcare providers to implement treatment strategies earlier in the disease process. This proactive approach is crucial for effectively managing rheumatoid arthritis, as early treatment can greatly enhance long-term outcomes and improve the quality of life for patients. Understanding the implications of a positive anti-CCP test empowers patients to take an active role in managing their health and making informed decisions regarding their treatment options.
Erythrocyte Sedimentation Rate (ESR): A General Indicator of Inflammation Levels
The erythrocyte sedimentation rate (ESR) is a non-specific marker commonly utilised in the UK to assess inflammation levels within the body. While it does not distinguish between types of arthritis, a high ESR can indicate the presence of inflammatory processes, rendering it a valuable tool when interpreted alongside other specific markers.
In practice, monitoring ESR is often employed to evaluate disease activity in patients with arthritis. A declining ESR may signal that inflammation is diminishing and that treatment is effective, while an increasing ESR could suggest a flare-up or worsening condition. Although this marker is not definitive on its own, it provides essential context when assessed alongside clinical symptoms and other test results. The ability to track ESR over time can help patients and healthcare providers comprehend treatment efficacy and adapt management plans accordingly, ensuring optimal health outcomes.
Expert Guidance on Interpreting Results from Arthritis Blood Tests
Understanding and interpreting arthritis blood test results is a complex process requiring careful consideration of various factors, including the specific markers tested and the patient's overall condition. An informed approach to interpreting these results can significantly impact treatment decisions and patient outcomes, ultimately shaping the trajectory of arthritis management.
Defining Normal Versus Abnormal Levels in Blood Tests
Establishing what constitutes normal and abnormal levels of arthritis blood test markers is not always straightforward. Each marker possesses its own reference range, which can vary based on factors such as age, sex, and laboratory standards. Understanding what defines normal can aid both patients and healthcare professionals in making informed decisions regarding diagnosis and treatment.
For instance, rheumatoid factor levels that fall within the normal range suggest that the autoimmune component of rheumatoid arthritis may not be present. Conversely, elevated levels may necessitate further investigation. Nevertheless, it is essential to recognise that a single test result should not dictate a diagnosis. Instead, healthcare providers must consider the entirety of a patient’s clinical presentation, incorporating symptoms, medical history, and results from other diagnostic tests to achieve a well-rounded understanding of the patient's health status.
Correlating Blood Test Results with Symptoms for Precise Diagnosis
Interpreting blood test results in the context of clinical symptoms is fundamental for achieving an accurate diagnosis and effective treatment plan. For example, a patient may exhibit elevated levels of certain markers yet not display any noticeable symptoms. In such scenarios, healthcare professionals may need to conduct further assessments to determine the relevance of the test results.
A comprehensive evaluation involves examining how blood test results correlate with pain levels, joint mobility, and other symptomatic indicators. For instance, if a patient shows high levels of anti-CCP antibodies but reports minimal symptoms, the healthcare provider might recommend a watchful waiting approach rather than immediate treatment. This correlation between laboratory results and clinical symptoms facilitates a more tailored and effective management strategy, enhancing the patient’s overall care and experience.
The Importance of Seeking Professional Guidance for Interpreting Test Results
In the UK, consulting healthcare professionals such as rheumatologists or general practitioners is vital for interpreting and acting on arthritis blood test results. These specialists have the expertise to contextualise test findings and recommend appropriate next steps. Patients are encouraged to engage in open discussions with their healthcare providers regarding their test results, as a collaborative approach can lead to a more thorough understanding of their condition.
Rheumatologists, in particular, can provide insights into the implications of specific markers and guide patients through the complexities of arthritis management. They may suggest additional tests or imaging studies to confirm a diagnosis or evaluate the extent of joint damage. Furthermore, having a clear grasp of the results can empower patients to make informed decisions about their treatment options and actively participate in their healthcare journey, fostering a sense of ownership over their health outcomes.
NHS Guidelines: Protocols for Effective Arthritis Blood Testing
The NHS plays a crucial role in guiding patients through the process of arthritis blood testing. Familiarity with these guidelines can help individuals understand when to seek testing and what to expect during the diagnostic journey, ensuring a smoother experience overall.
Identifying the Right Time to Undergo Testing for Arthritis
NHS guidelines advocate for conducting blood tests when patients exhibit symptoms indicative of arthritis, such as persistent joint pain, swelling, or stiffness. Early testing can facilitate timely diagnosis and intervention, ultimately improving long-term outcomes for those suffering from arthritis and enhancing their quality of life.
In specific circumstances, patients may be referred for testing by their GP when there is a suspicion of arthritis or if they are experiencing significant joint-related symptoms. Awareness of these guidelines empowers patients to advocate for themselves and seek the necessary testing to ensure they receive prompt and effective care, allowing for better management of their condition.
Determining the Optimal Frequency of Testing for Effective Management
The frequency of arthritis blood testing in the UK is typically dictated by the type of arthritis, the patient's condition, and the treatment plan. NHS guidelines suggest that regular testing may be essential for patients with active inflammatory arthritis to continuously monitor disease progression and treatment efficacy.
For instance, patients newly diagnosed with rheumatoid arthritis might undergo testing every few months during the initial treatment phase. Once the condition stabilises, the frequency of testing may be adjusted accordingly. Regular follow-ups with healthcare professionals ensure that testing schedules align with the patient's health status and treatment goals, facilitating optimal management and improved health outcomes.
Accessing NHS Testing Services for Comprehensive Arthritis Evaluation
Patients in the UK can access arthritis blood testing services through the NHS, typically requiring a referral from their GP. The process usually involves an initial consultation, during which the healthcare provider will assess symptoms and determine the necessity for testing. This systematic approach ensures that patients receive appropriate evaluations tailored to their specific needs.
Once referred, patients can expect to visit a local laboratory for blood collection. The results are typically processed and made available within a few days, allowing for timely decision-making regarding treatment options. Understanding how to access these services enables patients to navigate the healthcare system effectively, ensuring they receive the necessary evaluations promptly and efficiently.
Guidance on Interpreting Test Results within the NHS Framework
The NHS provides guidance on interpreting arthritis blood test results, which is essential for both patients and healthcare providers. Clear communication regarding test outcomes can significantly influence treatment decisions and enhance patient engagement in their care, ensuring that individuals understand their health status.
Healthcare professionals are trained to explain the significance of various markers and their implications for arthritis management. Patients are encouraged to ask questions and seek clarification to ensure they fully comprehend their results. This collaborative approach fosters a supportive environment for patients, enabling them to make informed choices about their health and treatment options, ultimately leading to enhanced patient satisfaction and improved outcomes.
Exploring Private Options for Arthritis Blood Testing in the UK
In addition to NHS services, private arthritis blood testing alternatives are available in the UK, providing patients with an alternative approach to accessing diagnostic evaluations. Understanding the benefits and considerations of private testing can empower individuals to make informed health decisions regarding their care and management strategies.
Key Benefits of Choosing Private Testing Services
Private testing for arthritis blood markers can offer numerous advantages, including expedited results and a more extensive range of tests. Patients opting for private testing often appreciate the reduced waiting times associated with private healthcare, facilitating quicker diagnoses and enabling timely adjustments to treatment plans.
Furthermore, private clinics may provide access to a broader array of tests, including specialised markers that are not typically included in standard NHS panels. This can be particularly beneficial for individuals seeking a more detailed assessment of their condition. The ability to receive prompt results and more in-depth testing can significantly enhance the overall patient experience and lead to better management of arthritis, fostering a sense of control over one's health.
Cost Considerations for Private Testing Services
While private arthritis blood testing presents distinct advantages, patients should be aware of the associated costs. Private testing can often be more expensive than NHS services, with prices that may vary considerably depending on the clinic and specific tests required.
Patients contemplating private testing are advised to conduct thorough research into their options and inquire about pricing before making a decision. Understanding the costs related to private testing can help individuals weigh the benefits against their budget, ensuring they make an informed choice that aligns with their healthcare needs and financial situation, ultimately enhancing their overall satisfaction with their care.
Selecting a Reputable Private Clinic for Accurate Blood Testing
Choosing a trustworthy private clinic for arthritis blood testing is crucial for ensuring accurate and reliable results. Patients are encouraged to seek clinics that are accredited and possess a proven track record in performing arthritis-related tests, ensuring that they receive high-quality care.
Reviews and recommendations from other patients can provide valuable insights into the quality of care offered by a private clinic. Additionally, healthcare professionals can assist patients in identifying reputable facilities that specialise in arthritis testing. Making an informed choice about where to undergo testing can significantly impact the quality of the patient experience and the reliability of the results obtained, ultimately contributing to better health outcomes.
Interpreting Results from Private Blood Tests for Informed Decision-Making
Interpreting results from private arthritis blood tests can be complex, necessitating discussion with a healthcare professional for clarity and context. Private clinics often provide detailed reports, which may encompass a multitude of markers and their corresponding levels; however, without proper context, these results can be challenging to interpret accurately.
Patients are encouraged to consult with their healthcare providers to fully grasp the significance of their test results and the implications for their treatment plans. This collaborative approach ensures that patients are well-informed and empowered to make educated decisions regarding their health, ultimately leading to improved management of their arthritis.
Technological Innovations in Arthritis Blood Testing: A Forward-Looking Perspective
The field of arthritis blood testing is continually evolving, with substantial advancements in technology and testing methodologies emerging in the UK. These innovations are transforming the way arthritis is diagnosed and managed, providing hope for more effective treatments and improved patient outcomes as research progresses.
Exploring New Markers and Innovative Testing Techniques
Recent advancements in arthritis blood testing technology include the development of new markers characterised by enhanced specificity and sensitivity. Researchers are actively investigating novel biomarkers that could yield insights into the underlying mechanisms of arthritis, potentially leading to earlier diagnoses and more targeted therapies tailored to individual patient needs.
Moreover, enhanced testing techniques, such as high-throughput assays and more sophisticated imaging technologies, are improving the accuracy of results and the ability to diagnose arthritis at earlier stages. These innovations empower healthcare providers to obtain more detailed information about a patient’s condition, thereby informing better treatment decisions and strategies tailored to individual needs and circumstances.
The Impact of Technological Advances on Diagnosis and Treatment Strategies
The influence of advancements in blood testing technology on diagnosis and treatment is profound and far-reaching. With the capability to identify specific markers associated with different types of arthritis, healthcare providers can personalise treatment plans to meet the unique needs of patients, leading to more effective management.
For instance, patients with early-stage rheumatoid arthritis may benefit from targeted therapies that focus on their specific biomarkers, thereby reducing the risk of joint damage and significantly improving long-term outcomes. The integration of new technologies into clinical practice promises to enhance the overall quality of care for patients, paving the way for more effective management of their conditions and improving their overall wellbeing.
Future Prospects for Advancements in Arthritis Blood Testing
The future of arthritis blood testing in the UK appears promising, with ongoing research and development aimed at further enhancing diagnostic capabilities and treatment options. As new markers and testing techniques continue to emerge, the potential for improved patient outcomes grows exponentially.
Continued investment in research is crucial for uncovering the complexities of arthritis and developing innovative solutions for diagnosis and treatment. By harnessing the power of advancing technologies, healthcare providers can better serve patients, ensuring they receive timely, accurate diagnoses and optimised treatment plans tailored to their unique needs, ultimately enhancing their quality of life.
The Connection Between Lifestyle Choices and Arthritis Blood Testing
While medical interventions are crucial in managing arthritis, lifestyle factors also play a significant role in overall health and wellbeing. Understanding how lifestyle choices can influence arthritis and recognising the importance of regular blood tests can empower patients to take control of their health journey, leading to better management and outcomes.
The Impact of Diet and Nutrition on Efficient Arthritis Management
Dietary choices can profoundly influence inflammation levels in the body, which is especially vital for individuals living with arthritis. Research indicates that certain foods, particularly those rich in omega-3 fatty acids, can help diminish inflammation and enhance joint health. Incorporating a balanced diet that includes a variety of fruits, vegetables, whole grains, and lean proteins can support overall wellbeing and potentially alleviate some arthritis symptoms, contributing to an improved quality of life.
Moreover, patients should collaborate closely with healthcare professionals, including dietitians, to devise personalised nutrition plans tailored to their specific needs and health objectives. Regular blood testing can also assist in monitoring nutrient levels and identifying any deficiencies that may be adversely affecting overall health, ensuring that dietary choices positively contribute to arthritis management and overall wellbeing.
Exercise and Physical Activity: Essential Components for Joint Health
Regular physical activity is paramount for managing arthritis and sustaining joint functionality. Engaging in low-impact exercises, such as swimming or walking, can help fortify the muscles surrounding the joints, enhance flexibility, and alleviate stiffness. Additionally, exercise provides further benefits by boosting overall physical and mental health, which is crucial for individuals dealing with chronic conditions.
Patients should consult with healthcare providers or physiotherapists to develop safe and effective exercise regimens customised to their individual capabilities and needs. By incorporating consistent activity into their lifestyles, patients can profoundly influence their arthritis management and elevate their overall quality of life, supporting their physical and emotional wellbeing.
Managing Stress for Optimal Health and Wellbeing
Stress can exacerbate symptoms of arthritis, making effective stress management strategies critical for patients. Techniques such as meditation, yoga, and deep-breathing exercises can help alleviate stress and enhance overall emotional wellbeing. By effectively managing their stress levels, individuals may experience improved symptoms and an enriched quality of life, contributing positively to their arthritis management.
Regular blood testing can also help identify any potential stress-related physiological changes within the body. By understanding how stress impacts their health, patients can implement effective stress management techniques into their daily routines, ultimately benefiting their arthritis management and overall health.
The Vital Importance of Open Communication with Healthcare Providers
Maintaining open communication with healthcare providers is essential for effectively managing arthritis. Patients should feel empowered to discuss their symptoms, concerns, and lifestyle choices candidly, as this collaborative approach can lead to more tailored and effective care that meets their individual needs.
Regular blood testing provides an opportunity for patients to engage in discussions about their health progress and treatment outcomes. By fostering a supportive relationship with healthcare professionals, patients can navigate the complexities of arthritis management with greater confidence, ensuring they receive the best possible care and support for their condition.
Adjusting Lifestyle Choices for Enhanced Health Outcomes
Ultimately, adopting a proactive approach to lifestyle changes can significantly improve the management of arthritis. By concentrating on diet, exercise, stress management, and open communication with healthcare providers, patients can greatly influence their health outcomes. Regular monitoring through blood tests can provide valuable insights into how lifestyle choices affect arthritis, empowering individuals to make informed decisions for their wellbeing and enhancing their overall health and quality of life.
Commonly Asked Questions About Blood Testing for Arthritis
What are the primary markers associated with arthritis blood tests?
Arthritis blood test markers are biological indicators present in the blood that aid in diagnosing and monitoring various types of arthritis by revealing signs of inflammation or autoimmune activity, which helps tailor treatment strategies effectively.
How are these markers utilised in the diagnostic process?
These markers are tested to assess the presence of arthritis and determine its type, assisting healthcare professionals in customising treatment plans based on specific findings and individual patient needs.
Why is regular testing crucial for arthritis patients?
Regular testing allows for ongoing monitoring of disease progression and treatment effectiveness, enabling timely adjustments to management strategies as required, which significantly enhances patient outcomes and quality of life.
What should I do if my blood test results are abnormal?
Consult your healthcare provider to discuss the implications of abnormal results and explore potential next steps in your arthritis management, ensuring a comprehensive approach to your care.
How often should I undergo blood testing for arthritis?
The frequency of testing varies depending on the type of arthritis and individual health status; your healthcare provider can recommend an appropriate schedule tailored to your specific needs and treatment goals.
What is the significance of rheumatoid factor in diagnosis?
Rheumatoid factor (RF) is an autoantibody indicating an autoimmune response, commonly used to diagnose rheumatoid arthritis and assess disease activity, aiding in informing treatment decisions.
Are there limitations to relying on blood testing for arthritis?
Yes, arthritis blood test markers can yield false positives or negatives and should be interpreted alongside clinical symptoms and other diagnostic tools for accuracy, ensuring a well-rounded understanding of the patient's condition.
Can lifestyle changes affect my arthritis blood test results?
Yes, lifestyle factors such as diet, exercise, and stress management can influence inflammation levels and overall health, ultimately impacting blood test results and informing treatment strategies.
What role does private testing play in arthritis management?
Private testing offers quicker results and potentially more comprehensive panels of tests, allowing for more tailored healthcare approaches to effectively managing arthritis and improving patient satisfaction.
How can I access NHS arthritis testing services?
NHS testing services can be accessed through GP referrals, where patients can undergo blood tests at local laboratories specifically for arthritis assessment, ensuring timely and effective care.
Connect with us on Facebook!
This Article Was First Found On https://bloodtest.co.uk
The Article: Arthritis Blood Test Markers Explained: Your Essential Guide appeared first on: https://ezbloodtest.com
The Article Arthritis Blood Test Markers: Essential Guide Explained Was Found On https://limitsofstrategy.com